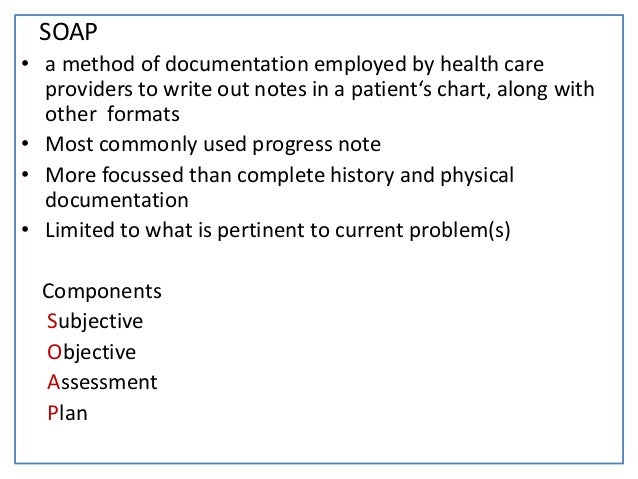
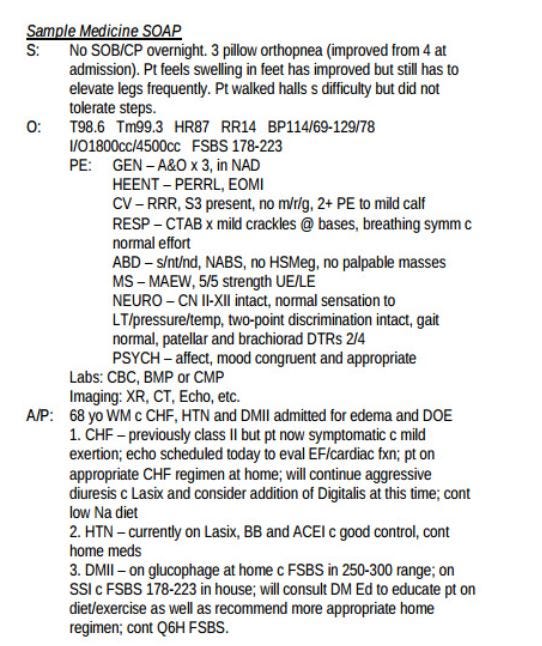
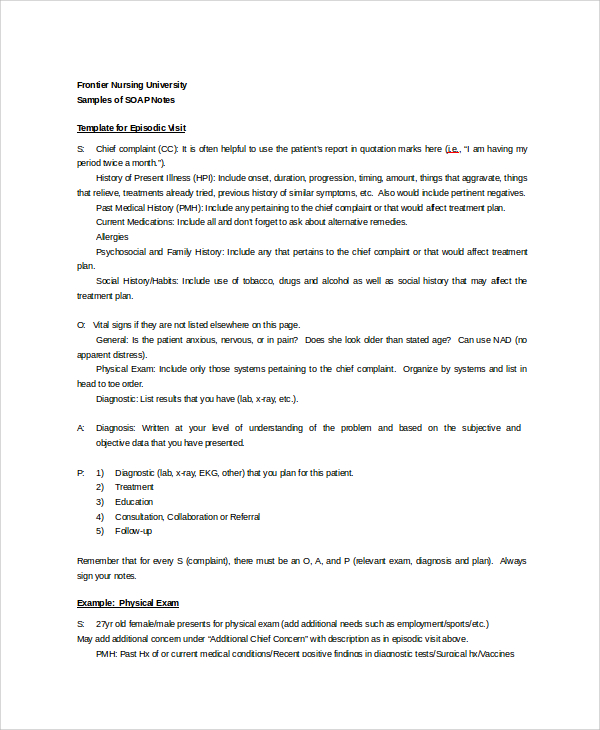
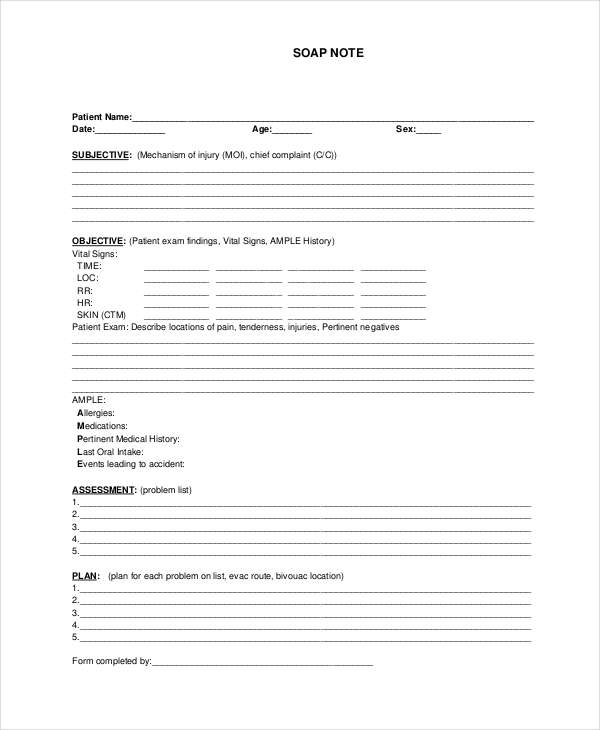
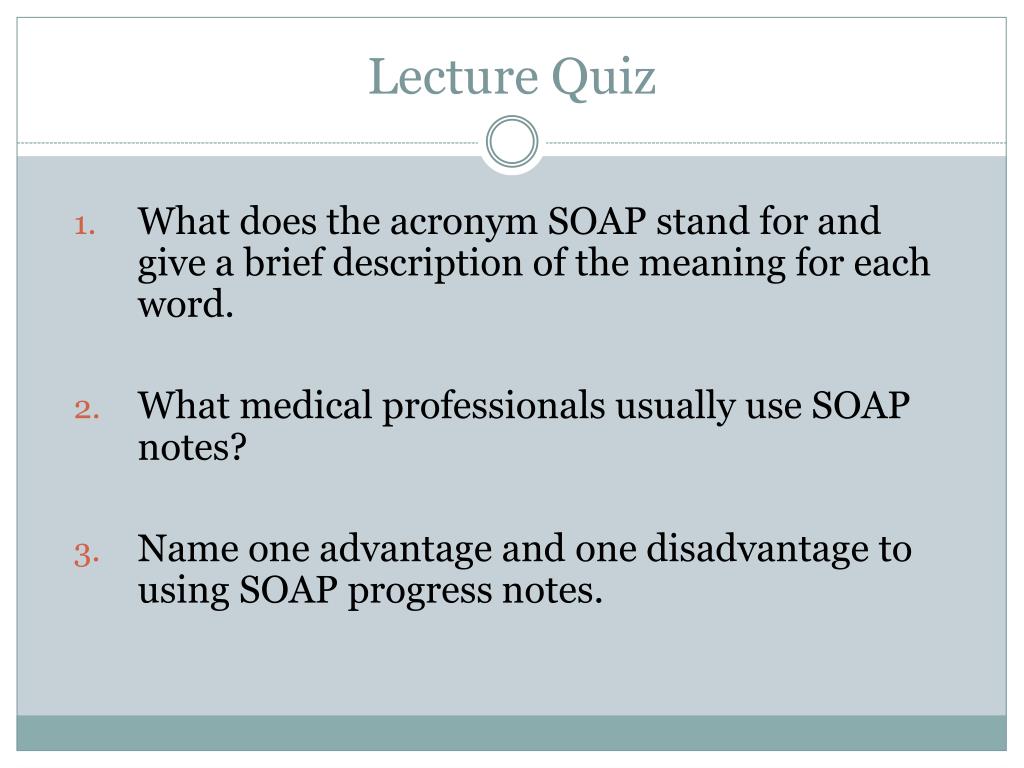
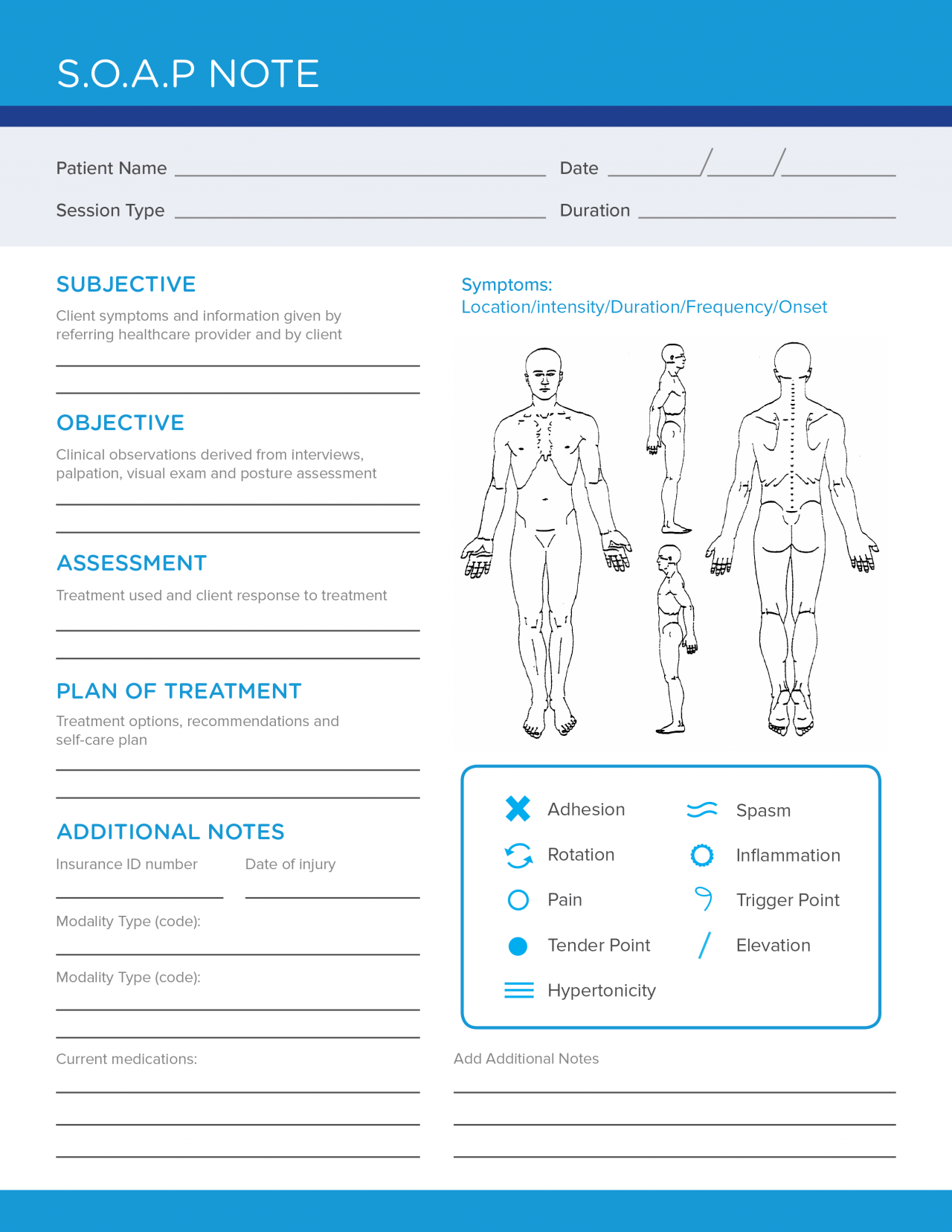
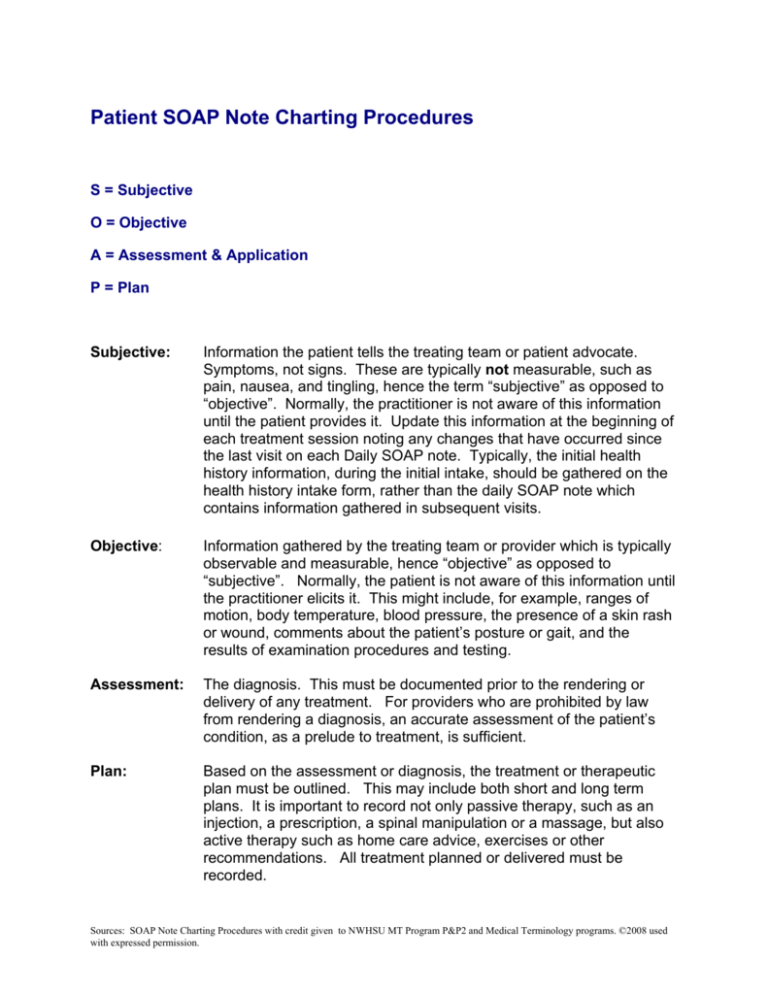
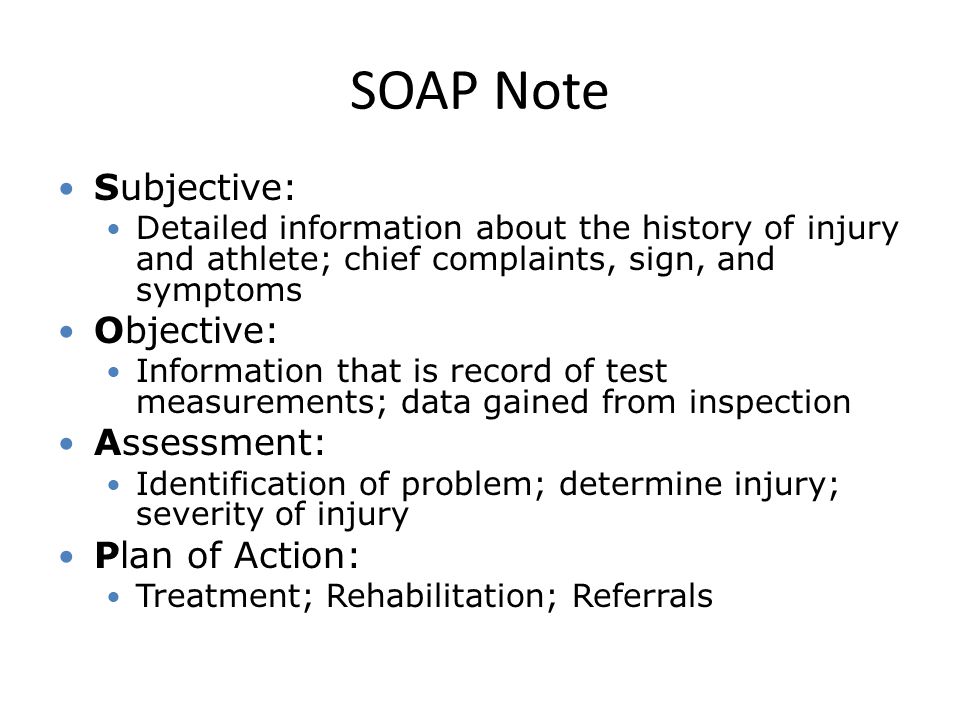
A SOAP note, or a subjective, objective, assessment, and plan note, contains information about a patient that can be passed on to other healthcare professionals To write a SOAP note, start with a section that outlines the patient's symptoms and medical history, which will be the subjective portion of the note After that section, record the patient's vital signs and Evidence in Integrative Healthcare In a previous post, we reviewed the necessity of basic best practices for SOAP notes including legibility, identification, and dated chart entries In this post, we review the proper structure and contents of a SOAP note The acronym SOAP stands for Subjective, Objective, Assessment, and PlanWho is the audience?

The Evolution Of Office Notes And The Emr The Caps Note Consult Qd
What does soap notes mean
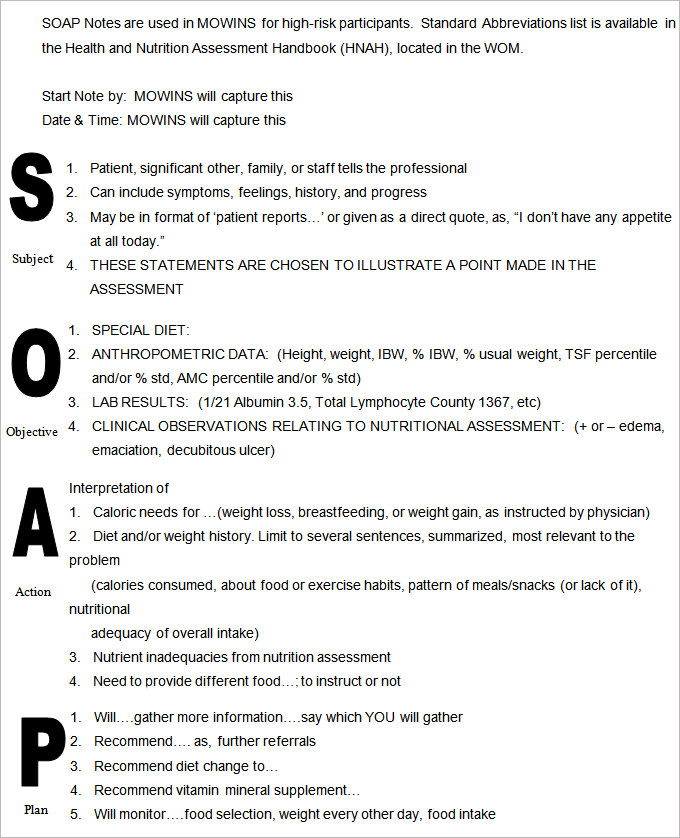
What does soap notes mean-Recovery SOAP NOTES abbreviation meaning defined here What does SOAP NOTES stand for in Recovery? SOAP (Subjective, Objective, Assessment, Plan) notes are an essential component of providing care and treatment for patients I t ' s vital to document data and information from every patient encounter T herapists must use SOAP notes to monitor and document patient progress, log services, and communicate patient information to other professionals




Soap Note How To Write Spotless Healthcare Notes Free Template Process Street Checklist Workflow And Sop Software
How to Write a SOAP Note What is a SOAP Note – Definition A SOAP note is a document usually used in the medical fraternity to capture a patient's details in the process of treatment This is one of the many formats that are used by professionals in the health sector The SOAP note is usually included in the patient's medical record for the purpose of informing any other health officerAnswer choices notes for others in healthcare to read notes for your coach to review notes for the patient to review notes for the public to review once posted online s Question 2 SURVEY seconds Q Which one is a form of observation? Meaning that there is a myriad of different ways to write a SOAP note, and one preceptor or supervising physician may want it a specific way versus another The biggest thing to remember is that SOAP notes are malleable and will change from provider to provider and from specialty to specialty But first, I want to share an example of both the first SOAP note I wrote in
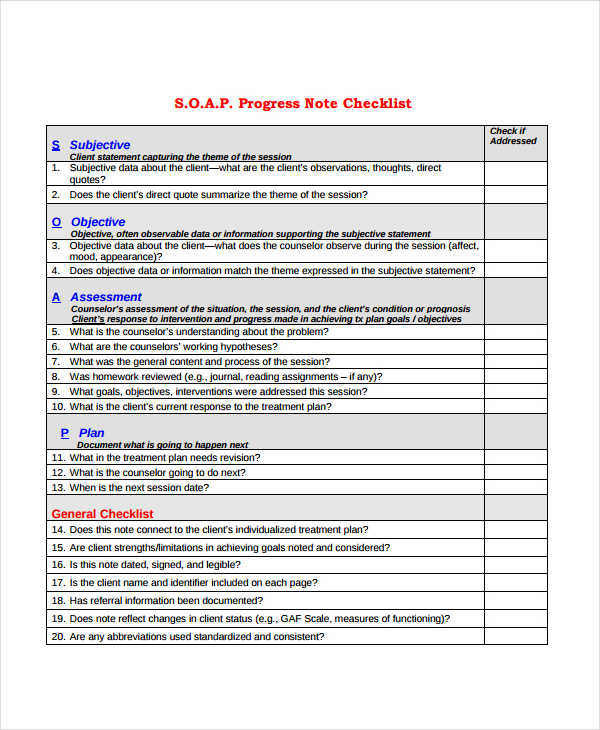
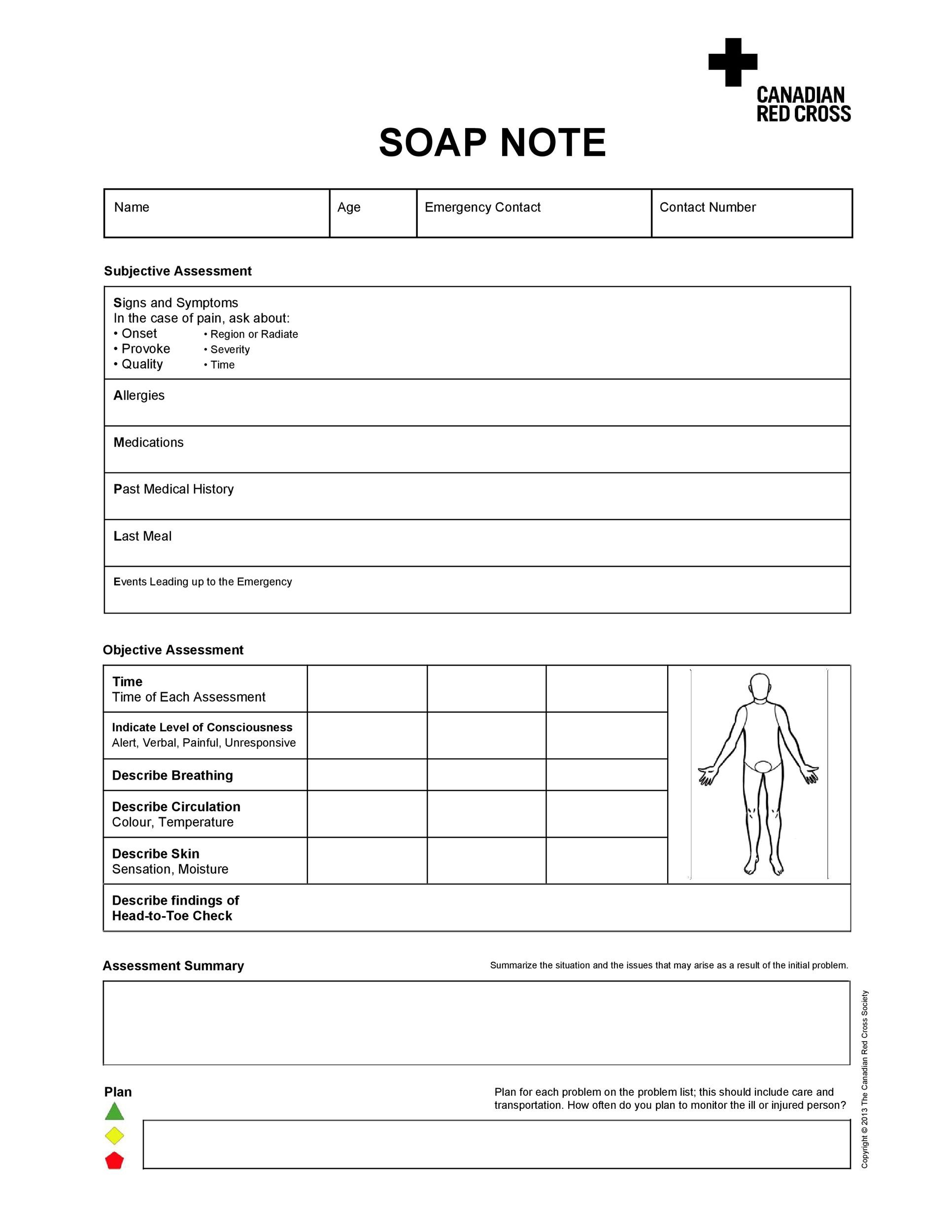
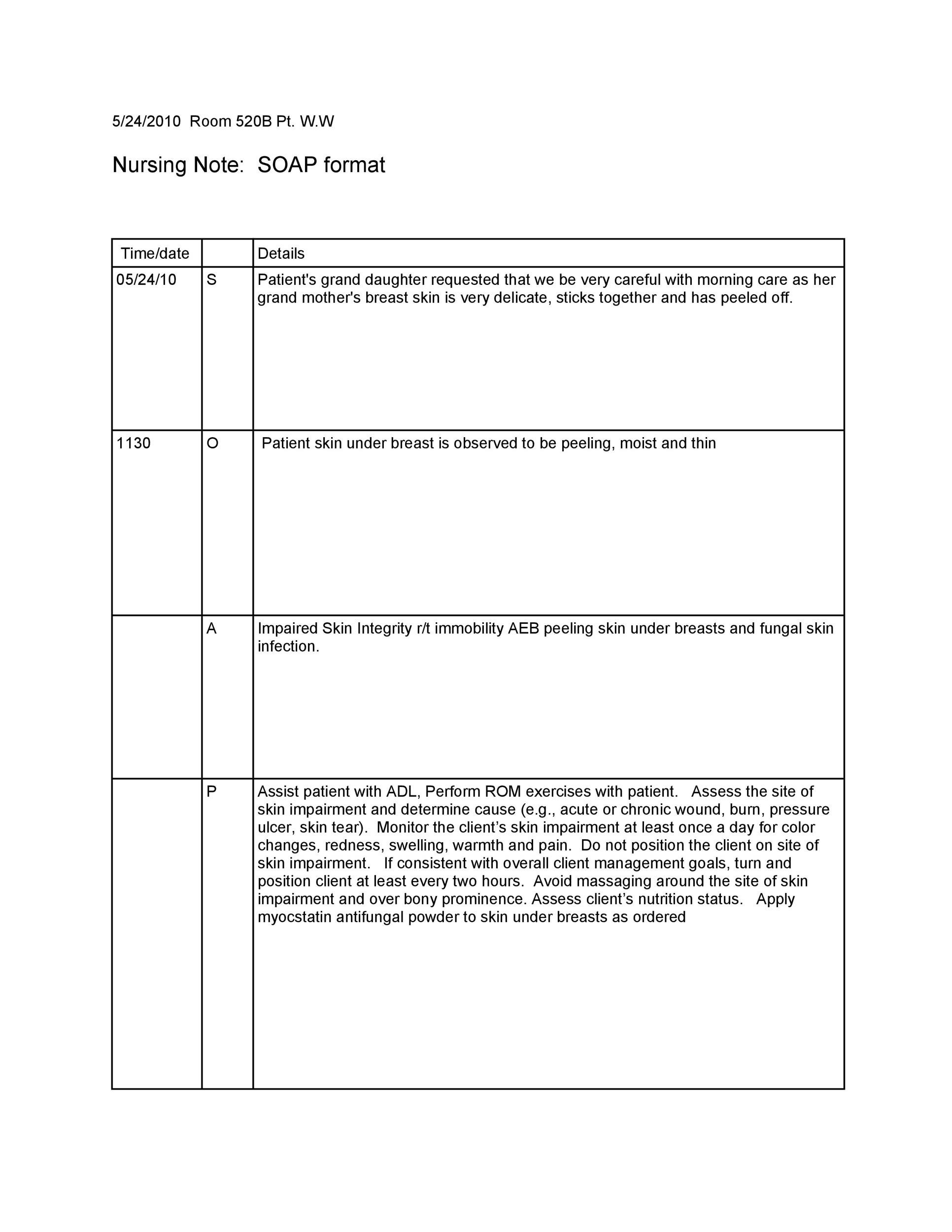
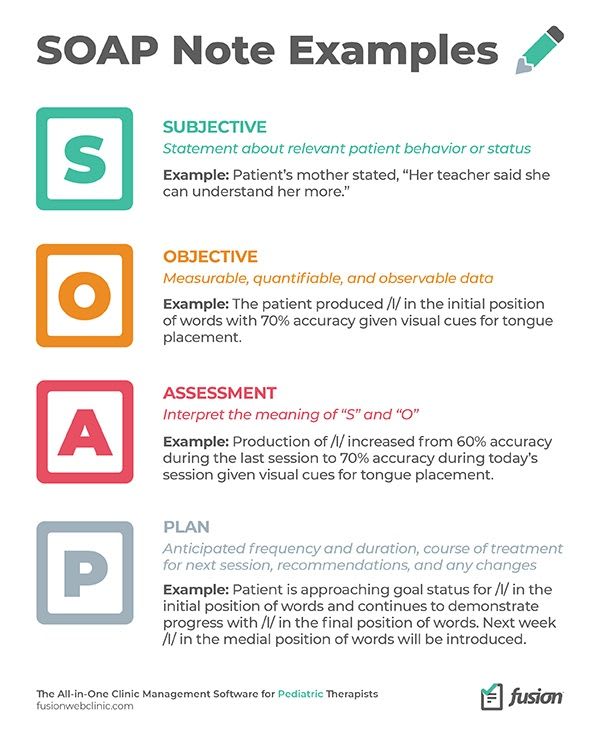
The SOAP Acronym SOAP is an acronym for the 4 sections, or headings, that each progress note contains Subjective Where a client's subjective experiences, feelings, or perspectives are recorded This might include subjective information from a patient's guardian or someone else involved in their care Objective For a more complete overview of a client's health A SOAP note is information about the patient, which is written or presented in a specific order, which includes certain components SOAP notes are used for admission notes, medical histories and other documents in a patient's chart SOAP Notes Pamela, APRN March, 1978 – 1130 pm After finishing walking rounds with the night shift nurse, I clocked out and sat down beside the chart rack to write notes on each of my five assigned patients before I went home I usually completed some of my assigned five patient charts during my shift, but with the nonstop evening, I barely
Toothnotes has some tips for you SOAP Notes Dentistry Example 1 Chief Complaint 23 year old male presents w/ a chief complaint of "my lower left back jaw has been sore for the past few days"S History of Present Illness Pt relates history of swelling for past 3 days, asymptomatic previously Medical History Med Conditions Medications Allergies Past Sx Social Hx Asthma Albuterol None Ear Lac 09 SOAP is an acronym Subjective, Objective, Assessment, and Plan This system was created to help prevent charting mistakes or information from being left out Just like each patient is unique, each chart in unique with information and length of notes Here is an example what each letter of SOAP includes




College Certificate Programs Certificateprograms Occupational Therapy Quotes Soap Note Occupational Therapy Activities




Documentation And Coding Practices For Risk Adjustment And Hierarchical Condition Categories
Busy practice with competing priorities and a commitment to that elusive worklife balance mean that you need to find the best, most efficient way of taking mental health progress notes Having worked with thousands of mental health practices over the years, we've picked up a couple of tips on how to effectively take SOAP notes These tips are going to make notetaking easier andDAILY PROGRESS NOTES SOAP Note Format soap notes meaning ,The term "SOAP notes" refers to a particular format of recording information regarding treatment procedures Documentation of treatment is an extremely important part of the treatment process In virtually *all* e mployment settings, some form of documentation is required and SOAP notes are theGet the top SOAP NOTES abbreviation related to Recovery




How Soap Notes Paved Way For Modern Medical Documentation




Free Soap Notes Templates For Busy Healthcare Professionals
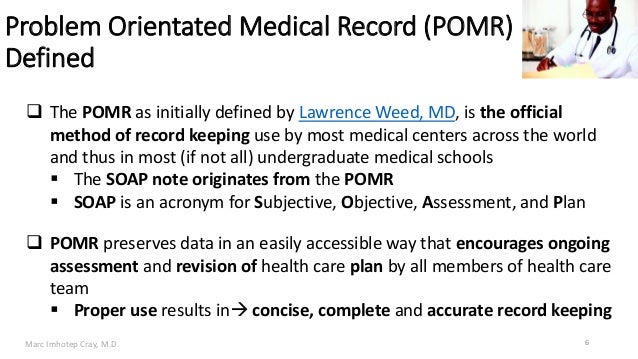
SOAP notes and other note formats Does it really matter?SOAP acronym for subjective data, objective data, assessment, plan, the way the progress notes are organized in problemoriented record keeping soap sōp any compound of one or more fatty acids, or their equivalents, with an alkali Soap is detergent and used as a cleanser green soap (medicinal soap) (soft soap) a soap made from vegetable oils other It stands for "Subjective Objective Assessment Plan," which provides documentation of a patient's condition, diagnosis and treatment SOAP notes were invented in the 1960s by Dr Lawrence Weed of the University of Vermont and didn't take long to enter widespread use in the medical profession



Counseling Soap Note Example Studocu



Free 18 Progress Note Examples Samples In Pdf Doc Examples
Occupational therapy SOAP notes, an overview of SOAP notes;What are SOAP notes? A DAP note is a method of documentation used by health care providers, social workers and similar professionals While SOAP is a more popular format in medicine, the Data, Assessment, Plan paradigm is potentially more appropriate for behavioral health The Basics of DAP



Progress Notes




Free Soap Notes Templates For Busy Healthcare Professionals
The SOAP note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by health care providers to write out notes in a patient's chart, along with other common formats, such as the admission noteDocumenting patient encounters in the medical record is an integral part of practice workflow starting with patient appointment scheduling, toDefinition of soap note in the Definitionsnet dictionary Meaning of soap note What does soap note mean?What does SOAP NOTES abbreviation stand for?




What Are Psychotherapy Notes Vs Progress Notes Theranest




Free Soap Notes Templates For Busy Healthcare Professionals
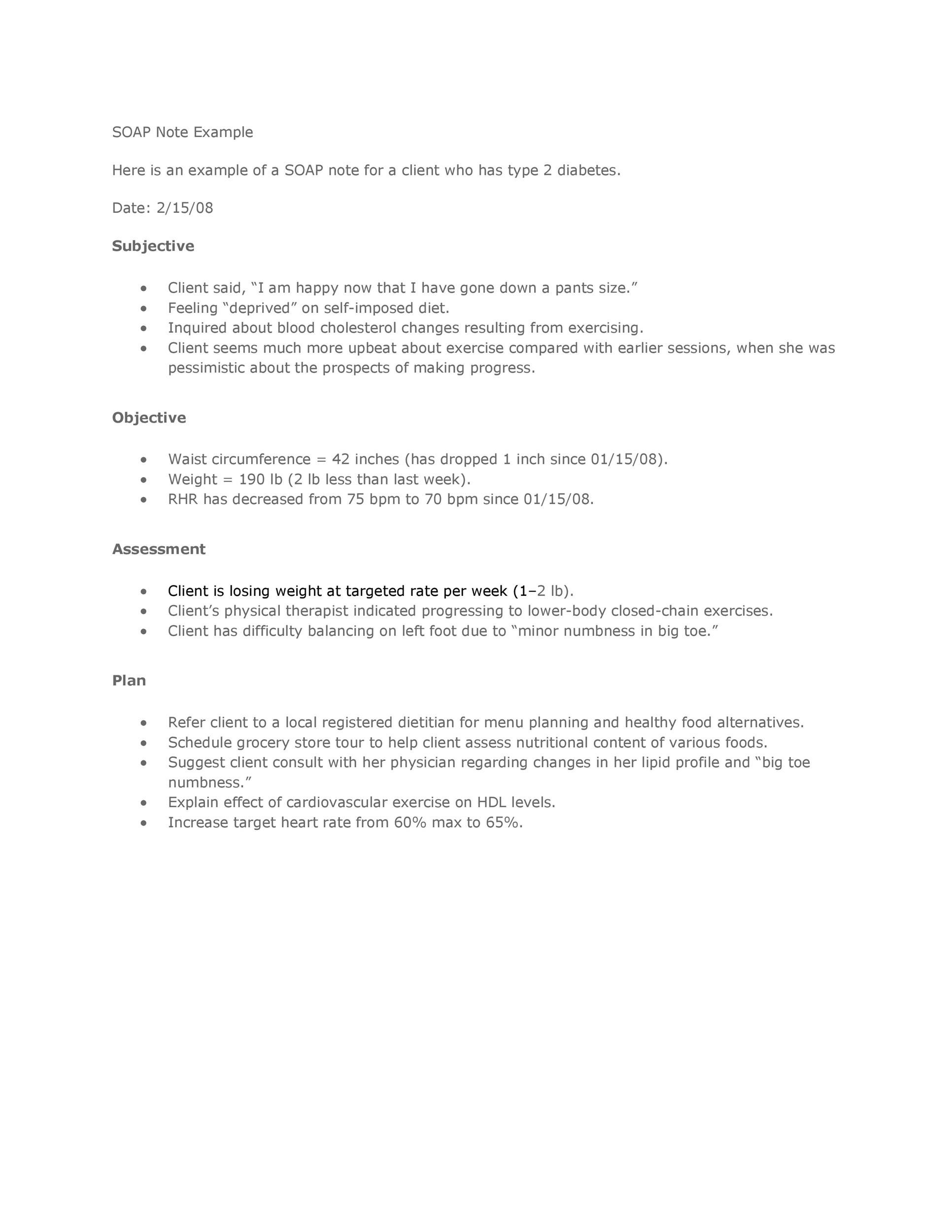
Information and translations of soap note in the most comprehensive dictionary definitions resource on the webSOAP notes include a statement about relevant client behaviors or status (Subjective), observable, quantifiable, and measurable data (Objective), analysis of the information given by the client (Assessment), and an outline of the next course of action (Planning) All SOAP notes should be kept in a client's medical record "SOAP notes have been used by therapists for decades," says Ann Zylstra, lead physical therapist at Evergreen Hospital in Kirkland, Washington She adds that personal trainers who use SOAP notes "facilitate the integration of personal trainers into a client healthcare team" According to the American College of Sports Medicine (ACSM), "The major benefit of this



Http Publichealth Lacounty Gov Sapc Healthcare Startods Sampleprogressnotesoap Pdf




Web Service Wikipedia
SOAP notes are the way you document that a client participated in and completed a session with you Depending on the billing process you have, a completed therapy note may also be the way a claim is generated Documentation also demonstrates your competency and shows how a client's needs have been addressedA SOAP note is basically a method of documentation that medical professionals employ to record a patient's progress during treatment Health care providers can use it to communicate the status of a patient to other practitioners, giving them a cognitive framework that they can refer to, upon assessment There are four components of the note, namely Subjective Upon medicalWhen confronted with a reading passage or document, students need a process to help them begin to determine the purpose or significance of the document It will then be much easier to interpret or even gather evidence from the document when students have a literacy tool to help them begin the process




Free Soap Notes Templates For Busy Healthcare Professionals




Soap Note How To Write Spotless Healthcare Notes Free Template Process Street Checklist Workflow And Sop Software
Sample Scenario Let's see how the nurse would write a SOAP note in this scenario Maria is a 56yearold, Hispanic female who just had her appendix SOAP notes are easy to use and designed to communicate the most relevant information about the individual They can also provide documentation of progress For clinical professionals, SOAP notes offer a clear, concise picture of where the client is at the time of each session They contribute to the continuity of care and are a tool for risk management and Complete your SOAP note with your plan 1 Create a list of all of the patient's medical problems Your problem list should be ordered by acuity 2 Propose a plan to manage each problem you've identified For example, if you're in the midst of treating a bacterial infection, indicate that you plan to continue antibiotics 3




Tips For Writing Better Mental Health Soap Notes Updated 21



Pomr And Soap Notes
SOAP notes provide a systemized way for healthcare providers to track and share information about patients' conditions and progress With the rise of Electronic Medical Record (EMR) systems, SOAP notes are becoming more important than in the past Chiropractic practices without EMR systems may have their own systems that would be difficult for people in otherSOAP notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible formats that could be used by a health professional They are entered in the patients medical record by healthcare professionals to communicate information to other providers of care, to provide evidence of patient contact and to inform theWhat does SOAP mean?



Understanding Clinical Notes This Article By Dot Health Medium




51 Sample Soap Notes In Pdf Ms Word Excel
Vague SOAP notes won't help you or your patient's care team, so take a few minutes to report any steps you plan to cover Finally, if you intend to modify your treatment, this is the section to note that A Physical Therapy SOAP Note Example Let's take a look at a detailed physical therapy SOAP note example We're quoting this one from the book " FunctionalSOAPS Why use SOAPS when interpreting Primary Source documents? The Subjective, Objective, Assessment and Plan (SOAP) note is an acronym representing a widely used method of documentation for healthcare providers The SOAP note is a way for healthcare workers to document in a structured and organized way This widely adopted structural SOAP note was theorized by Larry Weed almost 50 years ago




How To Write Massage Therapy Soap Notes Mblexguide



Http Www Drkney Com Videos k 11 Basic Progressnote Pdf
SOAP notes also create a paper trail of documentation that may be useful in the case of a malpractice suit More commonly, mental health SOAP notes are required for insurance reimbursements in the case of a thirdparty audit Switching to this notetaking technique is better for both your patients and your practice The SOAP framework can be incorporated into any notesThe SOAP notes, as discussed throughout this article, is a kind of medical note used by health care providers to accurately document and record patient's condition during treatment The SOAP note is one of the few documentations used by health care providers While the simple note is a note commonly used by many people to write down information so that they will not forget it This new and creative way to delve more deeply into your Bible reading allows you to record your thoughts, emotions, and how God speaks to you when studying scripture Let's look at how you can create SOAP notes for your journaling and bible study time S cripture Choose a Scripture to study or one that has special meaning to you




Soap Note How To Write Spotless Healthcare Notes Free Template Process Street Checklist Workflow And Sop Software




The Evolution Of Office Notes And The Emr The Caps Note Consult Qd
And an example of an occupational therapy SOAP note will be covered in this post The SOAP note method of documentation can be an excellent fit for theA SOAP note is a documentation format that massage therapists and other healthcare workers use to document client encounters SOAP is an acronym that stands for subjective, objective, assessment and plan In this post, I'll discuss what information goes inThe do's and don'ts of writing soap notes;




Soap Note




Birp Notes A Complete Guide On The Birp Note Taking Format
List of 1 best SOAP NOTES meaning form based on popularity Most common SOAP NOTES abbreviation full form updated in June 21A SOAP note (which stands for Subjective, Objective, Assessment, and Plan) is a document that's used by healthcare providers to create a patient's chart It's especially useful for assessing, diagnosing, and treating patients SOAP Notes make it easy to capture visit details for each client, retrieve history, and view progress Additionally, you can duplicate, add to, or edit client SOAP NotesIs there a repetition of words?




Soap Format Of Electronic Health Records Emrs For Veterinary Practices




Documentation Of Pharmaceutical Care Ppt Download
SOAP notes are a type of documentation which, when used, help generate an organized and standard method for documenting any patient data Any type of health professionals can use a SOAP note template – nurse practitioners, nurses, counselors, physicians, and of course, doctors Using these kinds of notes allows the main health care provider to collect information about aS– The S stands for Scripture you physically write out the scriptureyou'll be amazed that what God will reveal to you just by taking the time to slow down and actually write out what you are reading! SOAP is an abbreviation that is used to shorten the real name Before we explain what, each letter means, let us tell you the general definition of the SOAP note It is a type of document which is created for gathering patient's data relating to symptoms and diseases SOAP notes are needed to inform doctors and pediatricians about human health



How To Write A Soap Note Occupational Therapy




Pdf Clinical Note Taking Is Very Challenging For Many Students That Are Novice In The Field Many Times Even Professionals Ask What Type Of Note Taking Is Easy For You So I
What Are SOAP Notes in Counseling Physical Therapy Soap Note 1 file(s) 48 KB Download SOAP originated from another method of notetaking known as the POMR POMR or the problemoriented medical record was developed by Dr Lawrence Reed, a pioneer in the field of notetaking In the decades passed since its origins, SOAP has been used by uncountable healthcareToday, the SOAP note – an acronym for Subjective, Objective, Assessment, and Plan – is the most common method of documentation used by providers to input notes into patients' medical records They allow providers to record and share information A SOAP (s ubjective, o bjective, a ssessment, p lan) note is a method of documentation used specifically by healthcare providers SOAP notes are used so staff can write down critical information concerning a patient in a clear, organized, and quick way




4 Common Mistakes To Avoid When Writing Soap Notes Simplepractice
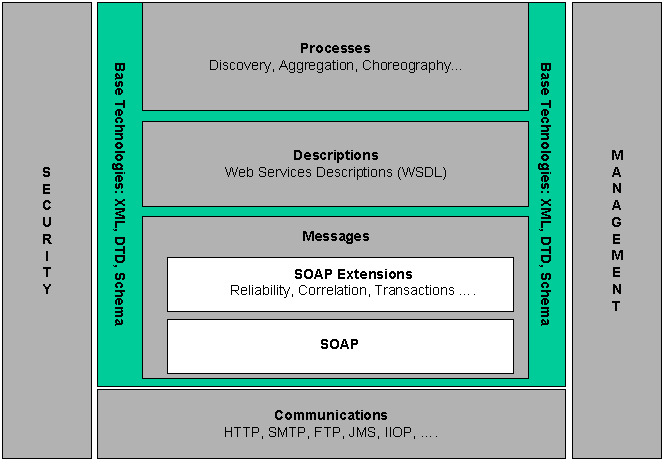



Web Services Architecture
Answer choices Objection Objective subjective assessment s Question 3 SURVEY seconds Q ThisQuestions to ask when writing each section;The benefits of using SOAP notes in occupational therapy;




Transitioning To Soap 2 0 Webpt Emr Help
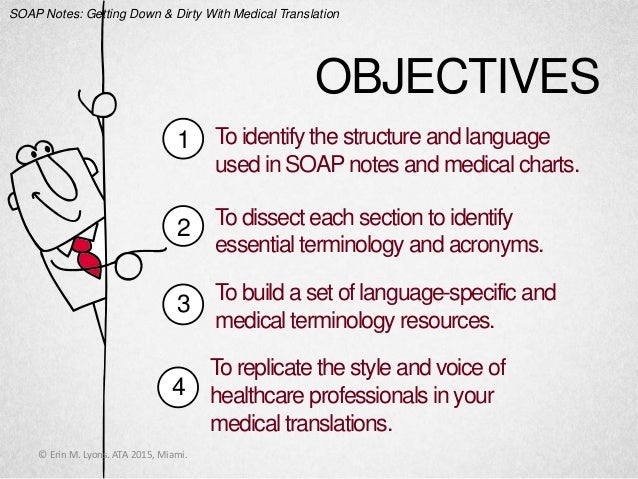



Soap Notes Getting Down And Dirty With Medical Translation
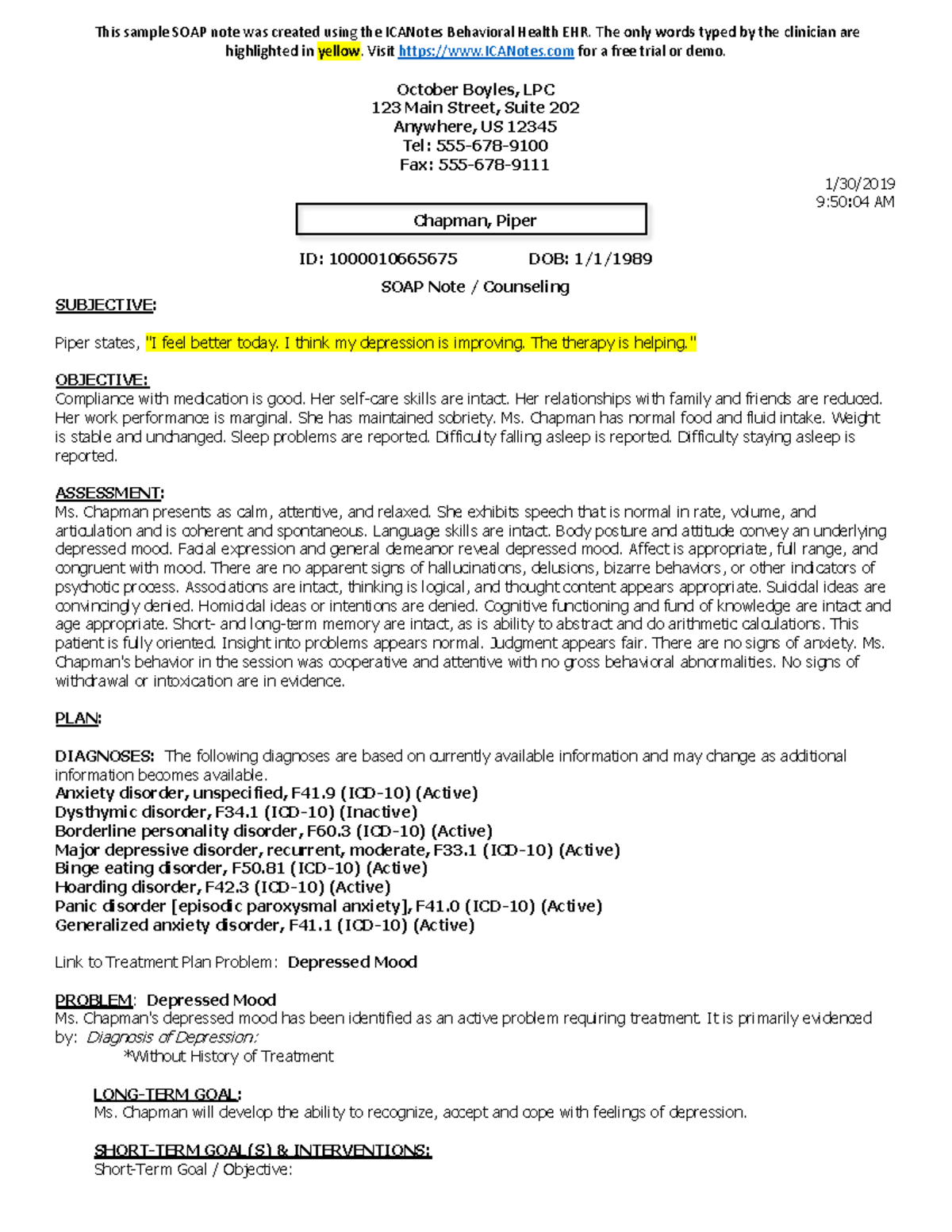
O– The O stands for observation what do you see in the verses that you're reading?A SOAP note to the inexperienced can seem very confusing and difficult to understand However when you break them down they become very simple A SOAP note is by definition a document used by nurses doctors and therapist along with other health counselors It is universally formatted so that all health care providers use the same templateS O A P NOTE S = Subjective or summary statement by the client Usually, this is a direct quote The statement chosen should capture the theme of the session 1 If adding your own explanatory information, place within brackets to make it clear that it is not a direct quote



40 Fantastic Soap Note Examples Templates ᐅ Templatelab



Soap Note Writing Tips For Mental Health Counselors Youtube




Soap Note How To Write Spotless Healthcare Notes Free Template Process Street Checklist Workflow And Sop Software




What Is A Soap Note Jess Brantner Wvu Dietetic Intern




Soap Note Flashcards Quizlet




How To Write Incredible Physical Therapist Soap Notes



Free 15 Soap Note Templates In Pdf Ms Word




Soap Note How To Write Spotless Healthcare Notes Free Template Process Street Checklist Workflow And Sop Software



40 Fantastic Soap Note Examples Templates ᐅ Templatelab




How To Write Incredible Physical Therapist Soap Notes




What Are Soap Notes In Counseling Examples




Understanding Soap Format For Clinical Rounds Global Pre Meds




Soap Notes The St John S Pa Program Survival Guide



Tips For Writing Better Mental Health Soap Notes Updated 21




Soap Notes Sample Medicine Soap A P Surgery Soap Pdf Free Download



Tips For Writing Better Mental Health Soap Notes Updated 21




Medical Terminology And Abbrev Pages 1 10 Flip Pdf Download Fliphtml5



Soap Note And Documentation Templates Examples Seniors Flourish



1



Free 28 Note Templates Examples In Pdf Doc Examples




Soap Notes Youtube
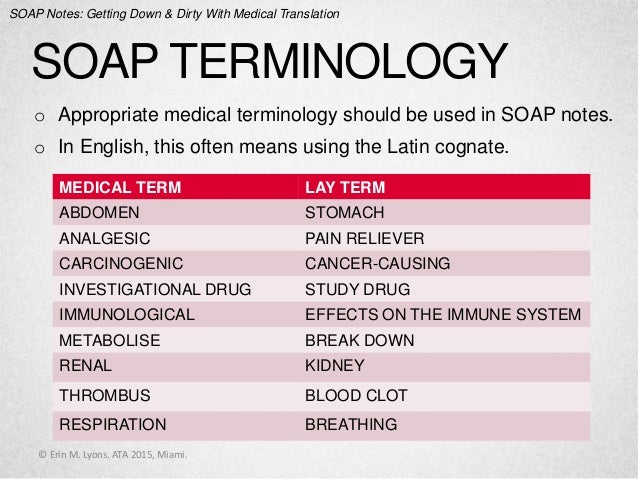



Soap Notes Getting Down And Dirty With Medical Translation
.png)



Free Massage Soap Notes Forms Massagebook




Soap 2 0 Faq Webpt Emr Help



1




Soap Note How To Write Spotless Healthcare Notes Free Template Process Street Checklist Workflow And Sop Software




Example Of Soap Note Soap Note Soap Notes Medical History




Nutritional Progress Notes Ppt Video Online Download




Client Intake Forms Agreements Acuity Scheduling



Physical Therapy Soap Note Example Therapy Daily Note




Free Soap Notes Templates For Busy Healthcare Professionals



Tips For Writing Better Mental Health Soap Notes Updated 21




How To Write Massage Therapy Soap Notes Mblexguide




Soap Notes Flashcards Quizlet




Soap Note Templates Safetyculture



Writing Pdf Line Page 4 For English Drymainjp Gearhostpreview Com



Tips For Writing Better Mental Health Soap Notes Updated 21



Soap Notes Counseling




Dietetics Nutritioncare Clinical Documentation 18 Ubc Wiki




Birp Notes A Complete Guide On The Birp Note Taking Format



Ppt Nutritional Progress Notes Powerpoint Presentation Free Download Id



40 Fantastic Soap Note Examples Templates ᐅ Templatelab



Help With Soap Note Development By Jasem James Fiverr




Dap Notes




What Are Soap Notes In Counseling Examples




Crafting The Ideal Ot Note Ot Potential



1



What Are Soap Notes In Counseling Examples




96 Best Soap Note Ideas In 21 Soap Note Speech And Language Therapy Activities



Health Science Self Guided Soap Notes Exploration By Laura Miller



Www Nbome Org Wordpress Wp Content Uploads 17 03 Comlex Usa L2pe Orientation Guide Website 19 Pdf
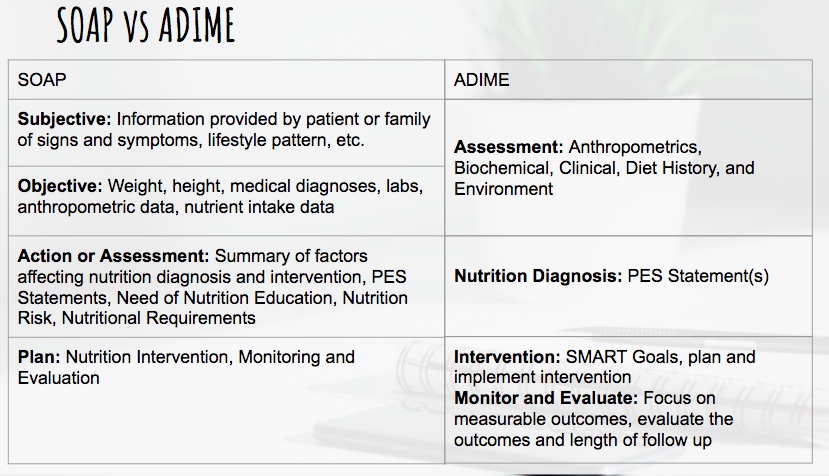



Dietetics Nutritioncare Clinical Documentation 18 Ubc Wiki




4 Common Mistakes To Avoid When Writing Soap Notes Simplepractice




Examples Of Soap Notes In Nursing Video Lesson Transcript Study Com



Soap Note How To Write Spotless Healthcare Notes Free Template Process Street Checklist Workflow And Sop Software




Soap Note How To Write Spotless Healthcare Notes Free Template Process Street Checklist Workflow And Sop Software



Physical Therapy Soap Note Example Therapy Daily Note



Soap Notes For Massage Therapy



1




What Is Soap Notes How Standardized Notes Improve Healthcare 5 Holland Irvine Ca Usa Cybernet Asia Cybernet Europe Cybernet Usa




Jm Rom Anatomical Terms Of Motion Musculoskeletal System



Patient Soap Note Charting Procedures




Free Soap Notes Templates For Busy Healthcare Professionals




The Evolution Of Office Notes And The Emr The Caps Note Consult Qd
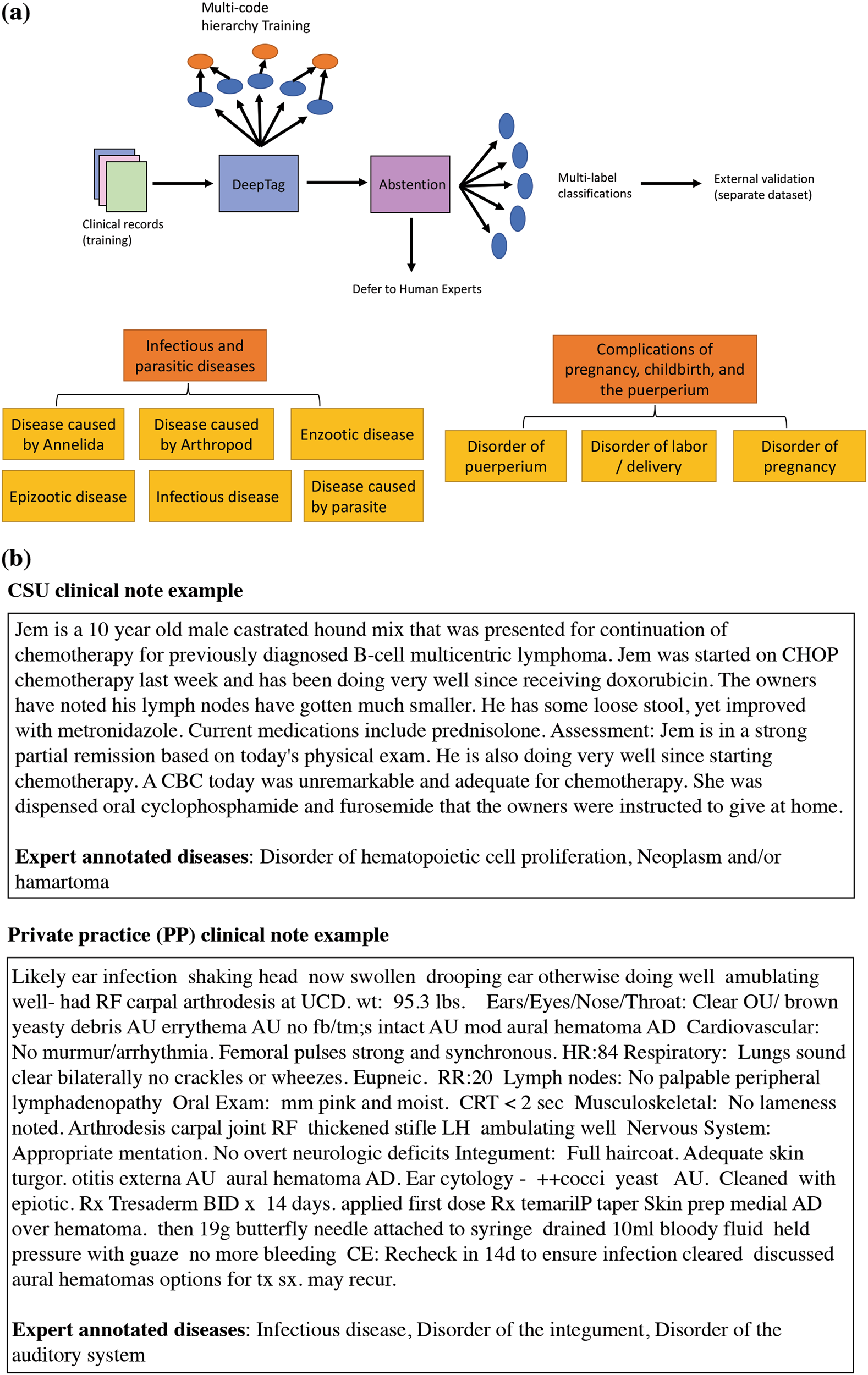



Deeptag Inferring Diagnoses From Veterinary Clinical Notes Npj Digital Medicine



Q7243zi2ui56wm




How To Write A Soap Note With Pictures Wikihow




How To Write Massage Therapy Soap Notes Mblexguide




Writing Samples




Academic Writing Guidelines
%20for%20veterinary%20practices.jpg)



Soap Format Of Electronic Health Records Emrs For Veterinary Practices



Evaluation Soap Notes Ppt Video Online Download



0 件のコメント:
コメントを投稿